 |
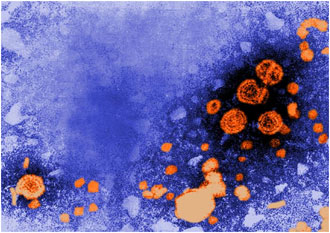 This transmission electron
micrograph (TEM) revealed the presence of hepatitis B virions.
The large round virions are known as Dane particles.
Photo courtesy of CDC/ Dr. Erskine Palmer.
This transmission electron
micrograph (TEM) revealed the presence of hepatitis B virions.
The large round virions are known as Dane particles.
Photo courtesy of CDC/ Dr. Erskine Palmer. High Risk Exposures
The healthcare setting can be a risky place
to work. During the provision of routine healthcare, there
exist high risk practices and procedures that are capable
of causing healthcare acquired infection with blood borne
pathogens.
More than 8 million U.S. healthcare workers
in hospitals may be exposed to blood or other body fluids
through the following types of contact (NIOSH, 2004):
- Percutaneous injuries (injuries through the skin) with
contaminated sharp instruments such as needles and scalpels
(82%)
- Contact with mucous membranes of the eyes, nose, or mouth
(14%)
- Exposure of broken or abraded skin (3%)
- Human bites (1%)
The revised New York State syllabus for the
Mandatory Infection Control training identifies high risk
practices and procedures capable of causing healthcare acquired
infection with bloodborne pathogens:
- Percutaneous exposures
- Other sharps injuries
- Mucous membranes and non-intact skin exposures
- Parenteral exposure.
Percutaneous exposures occur through handling/disassembly/disposal/reprocessing
of contaminated needles and other sharp objects. This can
occur through manipulating contaminated needles and other
sharp objects by hand (e.g., removing scalpel blades from
holders, removing needles from syringes, or recapping contaminated
needles and other sharp objects using a two-handed technique),
or by delaying or improperly disposing (e.g., leaving contaminated
needles or sharp objects on counters/workspaces or disposing
in non-puncture-resistant receptacles) (NYSDOH, 2008; NIOSH,
2004).
Up to 800,000 percutaneous injuries may occur annually among
all U.S. healthcare workers (both hospital-based workers and
those in other health care settings). After percutaneous injury
with a contaminated sharp instrument, the average risk of
infection is 0.3% for HIV and ranges from 6% to 30% for HBV
(NIOSH, 2004). On a positive note, the CDC has reported no
new cases of occupationally-acquired HIV since 2001 (CDC,
2006).
During the period 1995-2000, there were 10,378 reported percutaneous
injuries among hospital workers (NIOSH, 2004). The devices
most associated with percutaneous injuries among hospital
workers during 1995-2000 were hypodermic needles (29% of injuries),
suture needles (17%), winged steel needles (12%), and scalpels
(7%). Other hollow-bore needles together accounted for 19%
of injuries, glass items for 2%, and other items for 14% (NIOSH,
2004).
During the period 1995-2000 there were 6,212 reported percutaneous
injuries involving hollow-bore needles in hospital workers.
Drawing blood from a vein (venipuncture) was responsible for
25% of percutaneous injuries involving hollow-bore needles
during 1995-2000, and injections were responsible for 22%
(NIOSH, 2004).
Recent research on a nationally representative sample utilizing
data from the US Bureau of Labor Statistics, identified registered
nurses as having the greatest frequency of needlestick injury
(Leigh, et al., 2008); while the occupations with greatest
risk of needlestick injury included biologic technicians,
janitors and cleaners, and maids and housemen.
Other means of sharps injury can occur when performing
procedures where there is poor visualization, such as: Blind
suturing, non-dominant hand opposing or next to a sharp, or
performing procedures where bone spicules or metal fragments
are produced.
Mucous membranes and non-intact skin exposures are
also a potential method for exposure to bloodborne pathogens.
Direct blood or body fluid contact with the eyes, nose, mouth
or other mucous membranes occurs through contact with contaminated
hands, contact with open skin lesions/dermatitis, or splashes/sprays
of blood or body fluids such as might occur during irrigation
or suctioning.
Parenteral exposures may occur through injection with
infectious material while administering parenteral medications,
sharing of blood monitoring devices such as glucometers, hemoglobinometers,
lancets, lancet platforms/pens, or through the infusion of
contaminated blood products or fluids.
Additional practice to prevent percutaneous exposures include:
- Avoid unnecessary use of needles and other sharp objects.
- Use care in the handling and disposing of needles and
other sharp objects.
- Avoid recapping unless absolutely medically necessary.
- When recapping, use only a one-hand technique or safety
device.
- Pass sharp instruments by use of designated "safe zones".
- A "safe zone" is an area such as a tray or basin
on the sterile field where an instrument is placed before
being picked up by a second person. This can prevent
"collision" injuries where OR personnel can be tuck
by another when passing instruments.
- Disassemble sharp equipment by use of forceps or other
devices.
- Modify procedures to avoid injury:
- Use forceps, suture holders or other instruments
for suturing.
- Avoid holding tissue with fingers when suturing or
cutting.
- Avoid leaving exposed sharps of any kind on patient
procedure/treatment work surfaces.
- Appropriately use safety devices whenever available:
- Always activate safety features. o Never circumvent
safety features.
Safe Injection Practices and Procedures
Outbreaks of healthcare-related bloodborne illness have occurred,
usually due to unsafe injection practices. Recent news headlines
that implicate specific healthcare organizations and specific
healthcare providers for unsafe injection practices shocked
the thousands of patients who may have had exposure to bloodborne
pathogens, but such practices and procedures also shocked
the broader healthcare community.
Injection safety or safe injection practices are a
set of measures taken to perform injections in an optimally
safe manner for patients, healthcare personnel, and others.
A safe injection does not harm the recipient, does not expose
the provider to any avoidable risks and does not result in
waste that is dangerous for the community. Injection safety
includes practices intended to prevent transmission of bloodborne
pathogens between one patient and another, or between a healthcare
worker and a patient, and also to prevent harms such as needlestick
injuries.
The investigation of four large outbreaks of HBV and HCV
among patients in ambulatory care facilities in the United
States identified a need to define and reinforce safe injection
practices (CDC, 2008b). The four outbreaks occurred in a private
medical practice, a pain clinic, an endoscopy clinic, and
a hematology/oncology clinic. The pain clinic was located
on Long Island, New York. The primary breaches in infection
control practice that contributed to these outbreaks were:
- reinsertion of used needles into a multiple-dose vial
or solution container (e.g., saline bag) and
- use of a single needle/syringe to administer intravenous
medication to multiple patients.
In one of these outbreaks, preparation of medications in
the same workspace where used needle/syringes were dismantled
also may have been a contributing factor. These and other
outbreaks of viral hepatitis could have been prevented by
adherence to basic principles of aseptic technique for the
preparation and administration of parenteral medications.
These include the use of a sterile, single-use, disposable
needle and syringe for each injection given and prevention
of contamination of injection equipment and medication.
The unsafe practices above have resulted in the transmission
of bloodborne viruses, including hepatitis B and C viruses
to patients; as well as the notification of thousands of patients
of possible exposure to bloodborne pathogens and recommendation
that they be tested for hepatitis C, hepatitis B virus, and
HIV. Additionally, healthcare providers were referred to licensing
boards for disciplinary action and multiple malpractice lawsuits
were filed on behalf of patients.
Outbreaks related to unsafe injection practices indicate
that some healthcare personnel are unaware of, do not understand,
or do not adhere to basic principles of infection control
and aseptic technique. A survey of US healthcare workers who
provide medication through injection found that 1% to 3% reused
the same needle and/or syringe on multiple patients. Among
the deficiencies identified in recent outbreaks were a lack
of oversight of personnel and failure to follow-up on reported
breaches in infection control practices in ambulatory settings
(CDC, 2008b).
It is important for to remember that pathogens including
HCV, HBV, and human immunodeficiency virus (HIV) can be present
in sufficient quantities to produce infection in the absence
of visible blood. Bacteria and other microbes can be present
without clouding or other visible evidence of contamination.
The absence of visible blood or signs of contamination in
a used syringe, IV tubing, multi-dose medication vial, or
blood glucose monitoring device does NOT mean the item is
free from potentially infectious agents.
All used injection supplies and materials are potentially
contaminated and should be discarded.
Providers should maintain aseptic technique throughout
all aspects of injection preparation and administration, which
includes the following:
- Medications should be drawn up in a designated "clean"
medication area that is not adjacent to areas where potentially
contaminated items are placed.
- Use a new sterile syringe and needle to draw up medications
while preventing contact between the injection materials
and the non-sterile environment.
- Ensure proper hand hygiene before handling medications.
- If a medication vial has already been opened, the rubber
septum should be disinfected with alcohol prior to piercing
it.
- Never leave a needle or other device (e.g. "spikes")
inserted into a medication vial septum or IV bag/bottle
for multiple uses. This provides a direct route for microorganisms
to enter the vial and contaminate the fluid.
- Medication vials should be discarded upon expiration or
any time there are concerns regarding the sterility of the
medication.
- Never administer medications from the same syringe to
more than one patient, even if the needle is changed.
- Never use the same syringe or needle to administer IV
medications to more than one patient, even if the medication
is administered into the IV tubing, regardless of the distance
from the IV insertion site.
- All of the infusion components from the infusate to
the patient's catheter are a single interconnected unit.
- All of the components are directly or indirectly
exposed to the patient's blood and cannot be used for
another patient.
- Syringes and needles that intersect through any port
in the IV system also become contaminated and cannot
be used for another patient or used to re-enter a non-patient
specific multi-dose vial.
- Separation from the patient's IV by distance, gravity
and/or positive infusion pressure does not ensure that
small amounts of blood are not present in these items.
- Never enter a vial with a syringe or needle that has
been used for a patient if the same medication vial might
be used for another patient.
- Dedicate vials of medication to a single patient.
- Medications packaged as single-use must never be used
for more than one patient:
- Never combine leftover contents for later use;
- Medications packaged as multi-use should be assigned
to a single patient whenever possible;
- Never use bags or bottles of intravenous solution
as a common source of supply for more than one patient.
- Never use peripheral capillary blood monitoring devices
packaged as single-patient use on more than one patient:
- Restrict use of peripheral capillary blood sampling devices
to individual patients.
- Never reuse lancets. Consider selecting single-use lancets
that permanently retract upon puncture.
Safe injection practices as identified in the CDC's
Guideline for Isolation Precautions: Preventing Transmission
of Infectious Agents in Healthcare Settings 2007 include
the following recommendations apply to the use of needles,
cannulas that replace needles, and, where applicable intravenous
delivery systems (CDC, 2007):
- Use aseptic technique to avoid contamination of sterile
injection equipment.
- Do not administer medications from a syringe to multiple
patients, even if the needle or cannula on the syringe is
changed. Needles, cannulae and syringes are sterile, single-use
items; they should not be reused for another patient nor
to access a medication or solution that might be used for
a subsequent patient.
- Use fluid infusion and administration sets (i.e., intravenous
bags, tubing and connectors) for one patient only and dispose
appropriately after use. Consider a syringe or needle/cannula
contaminated once it has been used to enter or connect to
a patient's intravenous infusion bag or administration set.
- Use single-dose vials for parenteral medications whenever
possible.
- Do not administer medications from single-dose vials
or ampules to multiple patients or combine leftover contents
for later use.
- If multidose vials must be used, both the needle or cannula
and syringe used to access the multidose vial must be sterile.
- Do not keep multidose vials in the immediate patient
treatment area and store in accordance with the manufacturer's
recommendations; discard if sterility is compromised or
questionable.
- Do not use bags or bottles of intravenous solution as
a common source of supply for multiple patients.
Surveillance/Evaluation
Each year an estimated 385,000 needlesticks and other sharps-related
injuries are sustained by hospital-based healthcare personnel;
an average of 1,000 sharps injuries per day (NIOSH, 2008).
Healthcare providers who may be exposed to blood or other
potentially infected material are at risk, particularly if
they are exposed to contaminated needles or other contaminated
sharps that may cause injury. In addition to the surveillance
needed regarding the potential for injury to healthcare providers,
similarly, surveillance is used to identify factors related
to the 2 million HAIs per year.
Surveillance is defined as the ongoing, systematic collection,
analysis, interpretation, and dissemination of data regarding
a health-related event for use in public health action to
reduce morbidity and mortality and to improve health (CDC,
2007). Multiple agencies require ongoing evaluation of potential
hazards from bloodborne pathogens, including the Occupational
Safety and Health Administration (OSHA), the Centers for Disease
Control and Prevention (CDC), National Institute for Occupational
Safety and Health (NIOSH). In New York State, the Department
of Health and each individual healthcare organization or facility
has policies that support the safety of patients and healthcare
providers, as well as identifying how and to whom HAIs are
reported and analyzed.
A comprehensive standardized method for recording and tracking
percutaneous injuries and blood and body fluid contact is
the Exposure Prevention Information Network (EPINet). The
EPINet system consists of a Needlestick and Sharp Object Injury
Report and a Blood and Body Fluid Exposure Report, and software
programmed in Access®* for entering and analyzing the data
from the forms. (A post-exposure follow-up form is also available.)
Since its introduction in 1992, more than 1,500 hospitals
in the U.S. have acquired EPINet for use; it has also been
adopted in other countries, including Canada, Italy, Spain,
Japan and U.K (EPINET, 2008). With this system, the following
is available:
- Identify injuries that may be prevented with safer medical
devices.
- Share and compare information and successful prevention
measures with other institutions.
- Evaluate the efficacy of new devices designed to prevent
injuries.
- Target high-risk devices and procedures for intervention.
- Analyze injury frequencies by attributes like jobs, devices,
and procedures.
- Prepare monthly, quarterly, and annual exposure reports.
They can be accessed at http://www.healthsystem.virginia.edu/internet/epinet/about_epinet.cfm#What-is-EPINet.
While any sharp device can cause injury and has the potential
for disease transmission, some devices have a higher disease
transmission risk, such as hollow-bore needles. Other devices
have higher injury rates, such as butterfly-type IV catheters
and devices with recoil action, blood glucose monitoring devices
with lancet platforms/pens. It is important to identify the
settings in which exposures occur and the circumstances by
which exposure is more likely to occur.
Contiune to Element III,
Con't.
|
 |