 |
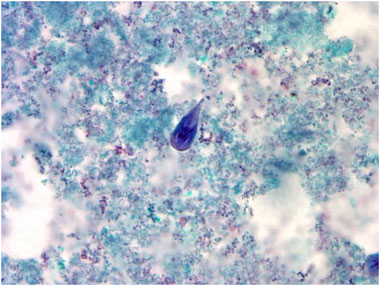
At a magnification of 1000X, this trichrome-stained
photomicrograph revealed the morphologic characteristics of
a blue-stained Giardia intestinalis protozoan trophozoite
(center).
Photo courtesy of CDC/ DPDx - Melanie Moser.
Personal protective equipment (PPE) is defined
by OSHA as specialized clothing or equipment worn by an employee
for protection against infectious materials. They are selected
based upon:
- Anticipated exposure type - splash/spray versus touch.
- Category of isolation precaution.
- Durability and appropriateness for the task.
- Fit.
As part of the Bloodborne Pathogen Standard, OSHA requires
employers to provide appropriate PPE for employees. Employers
must also ensure that PPE is disposed, or that reusable PPE
is cleaned, laundered, repaired and stored after use. OSHA
specifies the circumstances for which PPE is indicated; the
CDC recommends when, what, and how to use PPE (CDC, 2007).
Types of PPE
- Gloves - protect hands .
- Gowns/aprons - protect skin and/or clothing
- Masks and respirators - protect mouth/nose; respirators
protect respiratory tract from airborne infectious agents
- Goggles - protect the eyes
- Face shields - protect face, mouth, nose and eyes
There are four key points to remember about PPE use:
- First, don it before any contact with the patient is made,
generally before entering the room.
- Once the PPE is on, use it carefully to prevent spreading
contamination.
- When tasks have been completed, remove the PPE carefully
and discard it in the receptacles provided.
- Then immediately perform hand hygiene before going on
to the next patient.
Gloves
Gloves are used in patient care situations as well as for
environmental services. They are made of vinyl, latex, nitrile
and other materials. They are available in both sterile and
non-sterile forms; some are made for single use, others are
reusable. Healthcare workers sometimes wear a single pair
of gloves; sometimes double gloving is utilized (CDC, 2007).
|
The procedure for donning gloves is:
- Select correct type and size; use non-sterile for
isolation; select according to hand size.
- Insert hands into gloves.
- Extend gloves over isolation gown cuffs.
|
 |
Do's and Don'ts of Glove Use (CDC, 2007):
- Work from "clean" to "dirty"
- Limit opportunities for "touch contamination"
- Protect yourself, others and the environment:
- Don't touch your face or adjust PPE with contaminated
gloves.
- Don't touch environmental surfaces except as needed
during patient care.
- Change gloves
- During use if torn or heavily soiled (even when caring
for the same patient).
- After use on each patient.
- Discard in appropriate receptacle
- Never wash or reuse disposable gloves.
Gowns and Aprons
Gowns and aprons can be made of natural materials or synthetic
materials; they can be disposable or reusable; they vary in
level of fluid resistance; they can be sterile or clean. Three
factors influence the selection of a gown or apron. Firstly,
the purpose of its use must be considered. Isolation gowns
are generally the preferred PPE for clothing but aprons occasionally
are used where limited contamination is anticipated. If contamination
of the arms can be anticipated, a gown should be selected.
Gowns should fully cover the torso, fit comfortably over the
body, and have long sleeves that fit snuggly at the wrist.
Second are the material properties of the gown. Isolation
gowns are made either of cotton or a spun synthetic material
that dictate whether they can be laundered and reused or must
be disposed. Cotton and spun synthetic isolation gowns vary
in their degree of fluid resistance, another factor that must
be considered in the selection of this garb. If fluid penetration
is likely, a fluid resistant gown should be used.
The last factor concerns patient risks and whether a clean,
rather than sterile gown, can be used. Clean gowns are generally
used for isolation. Sterile gowns are only necessary for performing
invasive procedures, such as inserting a central line. In
this case, a sterile gown would serve to protect the patient
and the healthcare provider.
 |
The procedure for donning a gown is:
- Select appropriate type and size; fully cover torso
from neck to knees, arms to end of wrist and wrap
around the back;
- Opening is in the back;
- Secure at neck and waist;
- If gown is too small, wear 2 gowns:
- Gown #1 ties in front.
- Gown #2 ties in back.
|
 |
 |
The procedure for removing a gown is:
- Gown front and sleeves are contaminated;
- Unfasten ties at neck and then waist tie;
- Peel gown down away from neck and each shoulder
toward the same had;
- Turn contaminated outside to the inside;
- Hold removed gown away from body;
- Fold or roll into a bundle;
- Discard in appropriate receptacle.
|
 |
Face Protection
Masks protect the nose and mouth; they should fully
cover the nose and mouth and prevent fluid penetration. They
should fit snuggly over the nose and mouth, making masks with
flexible nose pieces that are secured to the head with string
ties or with elastic are preferable.
The procedure for applying a mask is:
- Pace over nose, mouth and chin;
- Fit flexible nose piece over nose bridge;
- Secure on head with ties or elastic;
- Fit snug to face and below chin;
- Adjust to fit.
|
 |
 |
For removal of a mask, use this procedure:
- Front of mask/respirator is contaminated - Do Not
Touch;
- Grasp only bottom tie first, then top tie/elastic
and remove;
- Discard in appropriate waste container.
|
 |
Goggles protect the eyes; personal prescription lenses
do not provide optimal eye protection and are NOT a substitute
for goggles. They should fit snuggly over and around the eyes;
antifog feature improves clarity.
Face shields protect the face, nose, eyes, mouth and
eyes; they should cover the forehead, extend below the chin
and wrap around side of face. When skin protection, in addition
to mouth, nose, and eye protection, is needed or desired,
for example, when irrigating a wound or suctioning copious
secretions, a face shield can be used as a substitute to wearing
a mask or goggles. The face shield should cover the forehead,
extend below the chin, and wrap around the side of the face.
Respiratory Protection
The purpose of respiratory protection is to protect workers
from inhalation of infectious aerosols (e.g. Mycobaterium
tuberculosis).
Types of respiratory PPE include:
- Particulate respirators,
- Half- and full-face elastomeric respirators,
- Powered air purifying respirators (PAPR).
The procedure for donning a particulate
respirator is:
- Select a fit tested respirator;
- Place over nose, mouth and chin;
- it flexible nose piece over bridge of nose;
- Secure on head with elastic;
- Adjust to fit;
- Perform a fit check:
- Inhale - respirator should collapse.
- Exhale - check for leakage around face.
|

|
|
|
|
|
|
Removing a particulate respirator entails the following
procedure:
- Lift the bottom elastic over your head first;
- Then lift the top elastic;
- Discard.
|
 |
Safe Work Practices
Key points about PPE:
- Don before contact with the patient, generally before
entering the room.
- Use carefully - don't spread contamination.
- Keep hands away from face;
- Work from clean to dirty;
- Limit surfaces touched;
- Change when torn or heavily contaminated;
- Remove and discard carefully, either at the doorway or
immediately outside the patient room; remove respirator
outside room.
- Immediately perform hand hygiene.
Sequence for donning PPE:
The order in which PPE is donned, is based on the combination
of needed PPE, although the following recommendations are
made, the specific situation will determine which sequence
is practical.
- Gown first,
- Mask or respirator,
- Goggles or face shield,
- Gloves.
Knowing the difference between "clean" and "contaminated"
areas of PPE is key to effective protection.
Contaminated areas include:
- The outside front of the PPE; and any
- Areas of the PPE that have had or are likely to have
been in contact with body sites, materials or environmental
surfaces where the infectious organism may reside.
Clean areas include:
- The inside, outside back, ties on head and back; and any
- Areas of PPE not likely to have been in contact with
infectious organisms.
The order in which PPE is removed also is important
in maintaining protection. The sequence is:
- Gloves,
- Face shield or goggles,
- Gown,
- Mask or respirator.
PPE is best removed at the doorway of the patient room. An
anteroom is ideally used; hand hygiene facilities (sink or
alcohol-based hand rub) are to be in this location, where
they will be needed.
Continue to Element
V
|
 |