|
Antiretroviral Medications
Prior to the advent of antiretroviral therapy (ART), also
called highly active antiretroviral therapy (HAART), HIV/AIDS
was considered a terminal disease. ART is an evolving field
of study with the focus on decreasing pill burden while maintaining
efficacy, development of new drug classes aimed at interfering
with viral replication at certain stages of the process, and
development of new drugs that are efficacious in the presence
of common mutations. Drug sequencing, the study of stepwise
medication use designed to decrease the likelihood of resistance
development to classes of drugs, has contributed to recommendations
for treatment and enhanced the overall understanding of resistance
development.
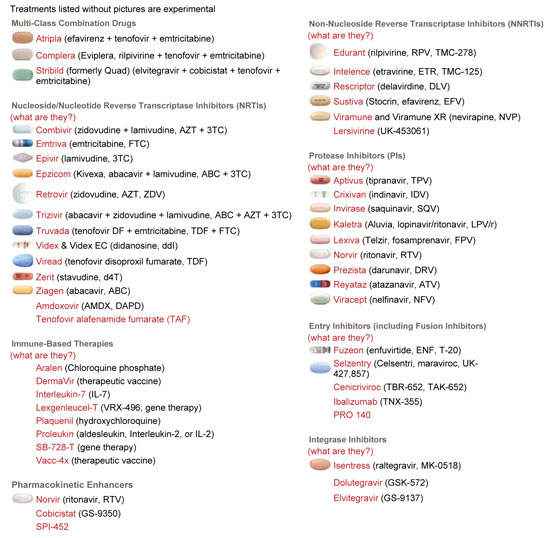
To date there are five classes of ART approved for use by
the FDA. These include:
- Non-nucleoside reverse transcriptase inhibitors (NNRTI);
- Nucleoside reverse transcriptase inhibitors (NRTI);
- Protease inhibitors (PI);
- Fusion inhibitors (FI) and Entry inhibitors; and
- Integrase inhibitors.
Each class was designed to interrupt the viral replication
cycle at a specific stage. In addition there are combination
pills that contain more than one medication: Combivir (ritonavir
and epivir), Truvada (tenofovir and emtriva), Epzicom (epivir
and abacavir), and Trizivir (ritonavir, epivir, and abacavir).
There are also multi-class combination medications, such as
Atripla (efavirenz, tenofovir, emtricitabine). The development
of drug combinations is aimed at improving adherence by decreasing
pill burden. Numerous other drugs are currently in clinical
trials.
The 2 newest classes of ART are:
Integrase Inhibitors
During the viral replication process, following reverse transcription,
the HIV DNA migrates into the nucleus of the cell. The integrase
enzyme facilitates incorporating viral genetic material into
the DNA of the cell. If this process is successful the CD4
cell produces HIV virus instead of other CD4 cells. The class
of integrase inhibitors is designed to interrupt this step
of the viral replication cycle.
Entry inhibitors
These drugs act by attaching themselves to proteins on the
surface of T-cells or proteins on the surface of HIV to prevent
the cells from binding together. The entry inhibitor can target
the gp120 or gp41 proteins on the HIV cell surface, or the
CCR5 or CXCR4 receptors on the surface of the CD4 cell. If
the medication is effective in preventing HIV from entering
the CD4 cell, the viral replication cycle is interrupted at
this stage.
Many other new and unique drugs are being developed and tested.
Several are expected to receive FDA approval later this year.
New classes of medications are especially helpful since they
are designed to work in the presence of existing viral mutations.
These medications, when available, will help to increase treatment
options, especially for persons who are highly treatment experienced.
Because medications for HIV treatment are updated regularly,
please consult those organizations who list current medications
used in the treatments for HIV/AIDS. One such website is:
http://www.aidsmeds.com/list.shtml.
Access to ART, adherence to the medical regimen, and response
to ART affect whether or when HIV progresses to AIDS.
However, not everyone with HIV infection benefits from the
new drug therapies. Many people cannot tolerate the unpleasant
or serious side effects from the medications. An estimated
40-50% of people with HIV who have access to the improved
medications are either unable to tolerate them or cannot adhere
to the complex treatment schedule. If a person cannot keep
this complicated schedule, the drugs do not work effectively
and viral resistance may develop.
Insurance programs and government programs for individuals
with low income pay for much of the cost of the HIV medicines
in the US. These medicines may cost several thousands of dollars
per person each month. People who live in other countries
where the medication is unaffordable have almost no access
to the newer therapies.
Although the new drug therapies work for many people to keep
the amount of virus in their bodies to very low levels, they
are not a cure for HIV. Once therapy is discontinued, viral
load may increase. Even during treatment, viral replication
may occur and the person remains infectious to others.
Many people find that after time, the virus becomes resistant
to the medication, and they must change medications. This
is especially true when the medications are not taken correctly,
and it limits the number of possible drug therapies that the
person might be able to use.
Side Effects of HIV Prescription
Medications
Patients often have unpleasant side effects when they use
prescription medications to treat their HIV infection. The
list of side effects includes:
- nausea
- diarrhea
- peripheral neuropathy (numbness in feet and hands)
- changes in body fat distribution called lipodystrophy,
with large fat deposits on the back of the neck, on the
stomach area and in breast size in women. This is usually
accompanied by a simultaneous, pronounced thinning of the
arms and legs.
- Interference with the metabolism of oral contraceptives
- osteoporosis
- diabetes or other changes in glucose metabolism
- damage to the nervous system, liver and/or other body
organs
People have used and relied on alternative, sometimes called
complimentary, therapies to treat HIV infection for as long
as HIV has been known. Many people use these treatments along
with therapies from their medical provider. Other people choose
to only use alternative therapies.
These therapies include a wide range of treatments, from
vitamins, massage, herbs, naturopathic remedies, and many
more. It is important for people who are taking alternative
therapies to tell their medical provider. There may be drug
reactions or other harmful side effects from the interactions
of the "natural" medicine and antiretrovirals.
Other drugs, including over the counter medications, prescription
medications and "street drugs," may have serious interactions
with antiretroviral medications. It is extremely important
that people on HIV medications tell their healthcare provider,
pharmacist or social worker about all other drugs they take.
Adherence
Taking antiretroviral (ART) medications at the right dose
and time has been shown to promote viral suppression and reduce
AIDS related mortality. Predictors of poor adherence have
not changed significantly over the past several years. Because
adherence often involves behavioral change, it is difficult
to implement and continue. Adherence is important for two
reasons: it affects the individual but also has a significant
effect on public health. People who are able to maintain an
undetectable viral load are less likely to progress to AIDS.
An undetectable viral load also decreases the probability
of viral transmission following an exposure.
In 2005 the media reported a case of multi-drug resistant
HIV in a person living in New York City. According to media
reports, the persons was recently diagnosed with HIV but had
so few treatment options that progression to AIDS was rapid.
Shet, et al. (2006) reported on the prevalence of ART resistant
mutations transmitted on a New York City cohort of recently
infected persons. Of the 112 people in the study, viral resistance
was identified among 25 % prior to beginning ART, while almost
10% had MDR strains of HIV. The increase of resistance was
statistically significant different between 1995-1998 and
2003-2004 (p=0.04).
The Importance of Access to Medical
Care
As the medications that are available to treat HIV infection
have become more numerous and complex, HIV care has become
a medical specialty. If possible, people who have HIV infection
should seek out a physician who is skilled in the treatment
of HIV and AIDS.
Despite the efforts of researcher who have worked for years
to develop a vaccine to prevent, or alleviate the severity
of HIV infection, there is currently no vaccine for HIV. No
one knows when a vaccine will be ready for distribution. Many
promising developments have been made and it is possible that
a vaccine will be available within this decade. Currently,
prevention is still the only way to avoid HIV infection.
Management of social issues plays a significant role in HIV
care. For this reason, an integrated team of professionals
is needed to meet the complex needs of patients with HIV.
Issues such as substance abuse, mental health, financial needs,
relationship issues, and housing can interfere with the patient's
ability to remain adherent to his medical care plan. Patient's
present to the clinic and report that they were unable to
take certain doses of medication because they had been instructed
to take it with food, but they had no food. Others report
missing appointments or tests because no transportation was
available. Specialists in the field now recognize the importance
of postponing initiation of ART if possible for persons with
chaotic life situations until changes can be made to optimize
the likelihood of treatment success. Referrals to community
based organizations, food pantries, and organizations managing
subsidized housing can greatly improve the possibility of
successful treatment.
|
Case Study
#6
|
|
Mr. S. came to the HIV clinic as a walk-in. He claimed
to be homeless, actively using drugs, and had no income.
He was diagnosed with HIV about eight years ago and
had been seen in different clinics on an intermittent
basis. He moved to this area about one year ago to attend
a rehab program, but relapsed and was living on the
street or in shelters when there was room. He took antiretroviral
therapy while he was in rehab, but had been out of all
HIV medications for at least three months. He noticed
thrush in his mouth and he has had a sore throat. He
wanted an urgent appointment to get a supply of medications.
The nurse explained to Mr. S. that he could be seen
by a provider as an urgent visit, and he would also
be seen by a social worker who would determine what
other urgent needs he had. After being assessed by both
staff members, the decision was made that the patient
appeared to be medically stable and would not need emergency
intervention. The plan was to obtain labs and past medical
records, and attempt to help the patient find stable
housing prior to restarting HIV medications. The social
worker contacted someone at the Department of Social
Services who agreed to provide an emergency housing
voucher for a nearby supported living program. Staff
at the program provided transportation to apply for
social services including food stamps and disability.
They took him to the food pantry and back to the HIV
clinic for his next appointment. Finally stabilized,
Mr. S. was able to keep his clinic appointments and
take his medications appropriately. He reconnected with
the rehab program and made arrangements to attend on
an out-patient basis. He has been clean and sober for
about four months. He is very appreciative of the support
he feels from his provider, social worker, and staff
at the clinic.
|
Continue on to Management
of HIV in the Healthcare Workplace
|