|
Because of the interrelationships between tuberculosis (TB)
sexually transmitted diseases (STD), HBV, HCV and HIV, a brief
discussion of each of these is included in this course, particularly
because of the impact of HIV on the co-infections, as well
as the impact of the co-infections on HIV.
Tuberculosis and HIV
Globally, there are probably 2 billion people (1/3 of the
world's population) infected with TB, and 8 million active
cases of TB each year. Tuberculosis is one of the leading
causes of death in the world.
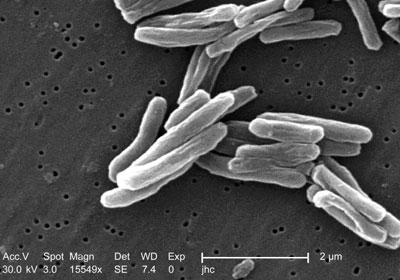
Photo Courtesy of the Public Health Image Library.
Mycobacterium tuberculosis (TB) is the bacteria that causes
tuberculosis. It is transmitted by airborne droplets from
people with active pulmonary or laryngeal TB during coughing,
sneezing, or talking. Although the TB bacteria can live anywhere
in the body, infectious pulmonary or laryngeal TB poses the
greatest threat to public health.
Latent infection, which is asymptomatic and not infectious,
can last for a lifetime. A presumptive diagnosis of active
TB is made when there are positive test results or acid-fast
bacilli (AFB) in sputum or other bodily fluids. The diagnosis
is confirmed by identification of M. tuberculosis on culture,
which should be followed by drug sensitivity testing of the
bacteria.
The TB bacteria are carried through the bloodstream and lymph
system, pumped through the heart, and then disseminated through
the body.
The largest amount of bacteria go to the lungs. In most
cases, this process, called primary infection, resolves
by itself and something called "delayed-type hypersensitivity"
is established. This is measured with the tuberculin skin
test. The incubation period for this primary infection is
two to 10 weeks. In most cases, a latent state of TB develops.
90% of people with latent TB never experience subsequent disease.
Other than a positive tuberculin skin test, people with latent
TB infection have no clinical, radiographic (x-ray), or laboratory
evidence of TB and cannot transmit TB to others.
Among the other 10% of infected individuals, the TB infection
undergoes "reactivation" at some time and they develop active
TB. About 5% of newly infected persons do so within the first
two years of primary infection and another 5% will do so at
some point later in life.
The period from time of initial exposure to conversion of
the tuberculin skin test is four to 12 weeks. During this
period, the patient shows no symptoms. The progression to
active disease and symptoms, such as cough, weight loss, and
fever, usually occurs within the first two years after infection,
but may occur at any time.
It is important to recognize the behavioral barriers to TB
management, which include deficiencies in treatment regimens,
poor client adherence to TB medications, and lack of public
awareness. Primary health care providers need adequate training
in screening, diagnosis, treatment, counseling, and contact
tracing for TB through continuing education programs and expert
consultation. Promoting patient adherence to the sometimes
complicated medication schedule, also requires consideration
of the patient's cultural and ethnic perceptions of his/her
health condition. Providing strategies and services that address
the multiple health problems associated with TB (such as alcohol
and drug abuse, homelessness, and mental illness) also builds
trust and promotes adherence to treatment plans.
Clinical trials have shown that daily preventive therapy
for 12 months reduces the risk for TB disease by more than
90% in patients with latent TB infection who complete a full
course of therapy. There is evidence that six months of preventive
therapy with Isoniazid may also prevent disease in approximately
69% of patients who complete the regimen. Every effort should
be made to ensure that patients adhere to this therapy for
at least six months. Children should receive at least nine
months of preventive therapy.
In order to prevent drug resistance and cure TB, the CDC
recommends that TB be treated with a multidrug regimen, which
may last six to 12 months. Current recommendations can be
found in the Kentucky Department of Health's Guidelines for
the Prevention, Treatment and Control of TB. A copy may be
obtained by calling the Kentucky Department of Health TB Program
at (502) 564-4276. Treatment of multidrug-resistant TB (MDR-TB)
is much more difficult and must be individualized. The patient
with MDR-TB requires treatment for two years or more.
TB/HIV Co-infection
HIV/TB co-infected persons are at considerably greater risk
of developing TB disease than those who only have TB. Studies
suggest that the risk of developing TB disease is 7% to 10%
each year for persons who are infected with both M. tuberculosis
and HIV, whereas it is 10% over a lifetime for a person infected
only with M. tuberculosis.
In an HIV-infected person, TB disease can develop in either
of two ways. A person who already has latent TB infection
can become infected with HIV, and then TB disease can develop
as the immune system is weakened. Or, a person who has HIV
infection can become infected with M. tuberculosis, and TB
disease can then rapidly develop because their immune system
is not functioning.
Pulmonary TB and extrapulmonary TB are among the conditions
included in the 1993 AIDS surveillance case definition. Any
HIV-infected person with a diagnosis of TB disease should
be reported as having TB and AIDS.
For more information on TB, contact:
- The communicable disease staff in each county health
department/district
- The Kentucky Department of Health TB program, (502) 564-4276
- The Centers for Disease Control and Prevention, Division
of TB Elimination website at http://www.cdc.gov/tb/default.htm.
Other Sexually Transmitted Diseases
and HIV
The term sexually transmitted disease (STD) is not specific
for any one disease, but refers to the more than 25 infectious
organisms that are transmitted through sexual activity and
the dozens of clinical syndromes that they cause. STDs affect
both men and women and can also be transmitted from mothers
to babies during pregnancy and childbirth. These may also
be called sexually transmitted infections (STIs).
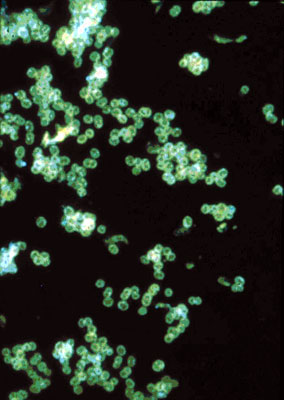
Fluorescent antibody-stained micrograph depicts
a positive result testing for the presence of gonorrhea.
Courtesy of Public Health Image Library.
Different bacteria cause STDs such as chlamydia,
gonorrhea and syphilis. Herpes, genital warts, hepatitis B
and HIV have different viral causes. Scabies are caused by
mites, and pubic lice cause "crabs." Trichomoniasis is caused
by tiny organisms called protozoa; "yeast" infections are
caused by fungi. STDs such as pelvic inflammatory disease
can have more than one cause - a woman may have both gonorrhea
and chlamydia causing this condition. A man may have more
than one cause for epididymitis.
In 1999, the World Health Organization estimated
that there were 340 million new cases of the four common curable
STDs (gonorrhea, chlamydia, syphilis and trichomoniasis) worldwide
among people age 15-49. Since the beginning of the AIDS epidemic,
researchers have noted the strong association between HIV
and other STDs.
Nationally, five of the top 10 most frequently
reported communicable diseases are STDs. In the US in 1999,
659,441 new cases of chlamydia were reported to the CDC. Reported
cases of gonorrhea rose to 360,076 in that year.
Primary and secondary cases of syphilis declined
to 6,657 cases. The Kaiser Family Foundation's website (www.kff.org)
lists estimates for incidence (new cases) and prevalence (total
number of cases) of both bacterial and viral STDs in the US,
noting that by age 24, at least one in three sexually active
people are estimated to have contracted an STD.
Primary STD infections may cause pregnancy-related
complications, congenital infections, infertility, ectopic
pregnancy, chronic pelvic pain and cancers. STDs can also
accelerate other infections like HIV.
HIV and STDs
The presence of infection with other STDs increases
the risk of HIV transmission because:
- STDs like syphilis and symptomatic herpes can cause breaks
in the skin, which provide direct entry for HIV;
- Inflammation from STDs, such as chlamydia, makes it easier
for HIV to enter and infect the body;
- HIV is often detected in the pus or other discharge from
genital ulcers from HIV-infected men and women;
- Sores can bleed easily and come into contact with vaginal,
cervical, oral, urethral and rectal tissues during sex;
- Inflammation appears to increase HIV viral shedding and
the viral load in genital secretions.
STDs are transmitted in the same way that HIV is transmitted:
by anal, vaginal and oral sex. In addition, skin-to-skin contact
is important for the transmission of herpes, genital warts,
syphilis, scabies and pubic lice.
In the past there was a great emphasis on symptoms as indicators
of STD infection. Research has changed this. We now know that
80% of those with chlamydia, 70% of those with herpes and
a great percentage of those with other STDs have no symptoms,
but can still spread the infections.
Along with prompt testing and treatment for those who do
have symptoms, the emphasis in the U.S. is screening for infection
based on behavioral risk. Patients cannot assume that their
health care providers do STD testing. In other words, women
who are getting a pap test or yearly exam should not just
assume that they are also being tested for chlamydia or any
other STD.
The following steps will help prevent STD infection:
- Abstain or be in a mutually monogamous relationship with
an uninfected partner.
- Know that many STDs have no symptoms.
- Know that birth control pills and shots do not prevent
infections - you must use condoms along with other birth
control methods.
- Go with your sex partner(s) for tests.
- Avoid douching.
- Learn the right way to use condoms and then use them correctly
and consistently every time you have sex.
- Be sure all sex partners are examined and treated if an
STD occurs.
- Change the ways you have sex so that there is no risk
of infection.
- Learn how to talk about correct use of condoms with all
sex partners.
- Practice the prevention you have learned for HIV and hepatitis.
At some sites, new urine LCR tests for some STDs are available.
Western Blot blood tests for herpes and hybrid capture tests
for genital warts may also be available. In most places, however,
cultures, wet preps and blood draws for syphilis remain the
standard testing method. It is vital that women get pap tests,
and that both men and women disclose a history of STD during
medical workups.
STD treatment is based on lab work and clinical diagnosis.
Treatments vary with each disease or syndrome. Because of
developing resistance to medications for some STDs, check
the latest CDC treatment guidelines.
Hepatitis B and HIV
Hepatitis is the inflammation of the liver that may be caused
by many things, including viruses. Current viruses include
Hepatitis A (not usually sexually transmitted or transmitted
by blood), B, C, D and others.
Hepatitis B (HBV) is a virus that is transmitted by the blood
and body fluids of an infected person. A vaccine to prevent
HBV is available. It is taken in a series of three injections
over 6 months. More than 90% of people who take the 3 injections
become immune to HBV.
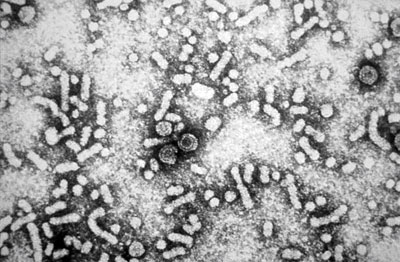
Hepatitis B virus under electron microscope.
Courtesy of Public Health Image Library.
HBV vaccine is relatively inexpensive for infants
and children. The adult doses are more expensive (costing
about $150 per person.) This cost is the likely reason that
most adults are not vaccinated against HBV.
Each year in the U.S. an estimated 200,000-300,000
people become infected with HBV. Of these, about 10% of adults
will become chronically infectious carriers of the virus.
There are 1,250,000 carriers of HBV in the U.S.
Each year, over 11,000 people will be hospitalized
and about 4,000-5,000 people will die in the U.S. from chronic
liver disease or liver cancer caused by HBV. HBV is transmitted
the same way as HIV, through sexual intercourse and sharing
needles. HBV is much more concentrated in blood, and it is
more infectious than HIV.
HBV is not transmitted by:
- Breastfeeding
- Sneezing
- Hugging
- Coughing
- Sharing eating utensils or drinking glasses
- Food or water
- Casual contact
Unvaccinated people are at higher risk for getting HBV if
they:
- Share injection needles/syringes and equipment;
- Have sexual intercourse with an infected person;
- Work where they come in contact with blood or body fluids,
such as in a health care setting, prison, or home for the
developmentally disabled;
- Use the personal care items (razors, toothbrushes) of
an infected person;
- Are on kidney dialysis;
- Were born in a part of the world with a high rate of Hepatitis
B (China, Southeast Asia, Africa, the Pacific Islands, the
Middle East, South America and Alaska).
The average incubation period for HBV is 120 days. People
are infectious when they are "Hepatitis B surface antigen
positive" (HbsAg) either because they are newly infected,
or because they are chronic carriers.
Most people recover from their HBV infection and do not become
carriers. Carriers (about 10% of adults who become infected)
have the virus in their body for months, years, or for life.
They can infect others with HBV through their blood or other
body fluid contact.
HBV causes damage to the liver and other body systems, which
can range in severity from mild, to severe, to fatal. Other
symptoms include:
- jaundice (yellowing of the eyes and skin)
- joint pain
- malaise
- dark urine
- nausea or vomiting
- skin rashes
Others who are infected with HBV experience more severe symptoms,
and may be incapacitated for weeks or months. Long-term complications
may also occur, and include:
- chronic hepatitis
- recurring liver disease
- liver failure
- cirrhosis (chronic liver damage)
A vaccine for HBV has been available since prior to 1990.
This vaccine is suitable for people of all ages, even infants.
People who may be at risk for infection should get vaccinated.
To further reduce the risk of or prevent HBV infection, a
person can:
- Abstain from sexual intercourse and/or injecting drug
use
- Maintain a monogamous relationship with a partner who
is uninfected or vaccinated against HBV
- Use safer sex practices (as defined in the Transmission
section)
- Never share needles/syringes or other injection equipment
- Never share toothbrushes, razors, nose clippers or other
personal care items that may come in contact with blood
- Use Universal or Standard Precautions with all blood
and body fluids
Infants born to mothers who are HBV carriers have a greater
than 90% reduction in their chance of becoming infected with
HBV, if they receive a shot of hepatitis B immune globulin
and hepatitis B vaccine shortly after birth plus two additional
vaccine doses by age six months.
It is vital that the women and their medical providers are
aware that the woman is a HBV carrier. People with HBV should
not donate blood, semen or body organs.
There is no cure for HBV. There are two approved drug treatments
for HBV, but these treatments do not cure, the virus. The
vaccine is not used to treat HBV infection once a person is
infected.
Hepatitis C and HIV
Hepatitis C is a liver disease caused by the hepatitis C
virus (HCV), which is found in the blood of persons who have
this disease. Hepatitis C is the leading cause of chronic
liver disease in the United States. Hepatitis C was discovered
in the late 1980s, although it was likely spread for at least
40-50 years prior to that.
Globally, 200 million people are infected with HCV. As of
1999, almost 4 million Americans, or 1.8% of the U.S. population,
have antibodies to HCV. This means that they have a current
or previous infection with the virus. About 3 million are
chronically infected, and the majority of them have some liver
damage.
The CDC estimates that as many as 1 million Americans were
infected with HCV from blood transfusions, and that 3.75 million
Americans do not know they are HCV-positive. Of these, 2.75
million people are chronically infected, and are infectious
for HCV. In the U.S., 8,000-10,000 deaths per year are attributed
to HCV-associated liver disease. The number of deaths from
HCV are expected to triple in the next 10-20 years.
HCV is transmitted primarily by blood and blood products.
Blood transfusions and the use of shared or unsterilized needles
and syringes have been the main causes of the spread of HCV
in the US. The primary way that HCV is transmitted now is
through injection drug use. Since 1992, all blood for donation
in the U.S. is tested for HCV.
The US Public Health Service estimates thaty the risk of
sexual transmission of HCV is approximately 5%, well below
the risk of sexual transmission of hepatitis B or HIV. If
a pregnant woman is infected with HCV, she may pass the virus
to her baby. However, this occurs in only about 5% of those
pregnancies.
Household transmission is possible if people share personal
care items such as razors, nail clippers, toothbrushes, etc.
HCV is not transmitted by:
- Breastfeeding.
- Sneezing.
- Hugging.
- Coughing.
- Sharing eating utensils or drinking glasses.
- Food or water.
- Casual contact.
The severity of HCV differs from HIV. The CDC states that,
for every 100 people who are infected with HCV:
- about 15% will fully recover and have no liver damage.
- 85% may develop long-term infection, and be infectious
for HCV.
- 70% may develop chronic liver disease.
- 20% may develop cirrhosis over a period of 20-30 years.
- 25% may die from the consequences of long term infection
(liver cancer or cirrhosis).
Persons with HCV may have few or no symptoms for decades.
When present, the symptoms of HCV are:
- Nausea and vomiting;
- Weakness;
- Fever;
- Muscle and joint pain;
- Jaundice (yellowing of the eyes and skin);
- Dark-colored urine;
- Tenderness in the upper abdomen.
There is no vaccine to prevent HCV infection. The following
steps can protect against HCV infection:
- Follow Universal and Standard Precautions to avoid contact
with blood or accidental needlesticks.
- Refrain from acquiring tattoos or skin piercings outside
of a legitimate business that practices Universal Precautions.
- Refrain from any type of injection drug use or drug equipment-sharing.
- Never share toothbrushes, razors, nail clippers or other
personal care items.
- Cover cuts or sores on the skin.
- Persons who are HCV-infected may use latex condoms and
practice safer sex to lower the small risk of passing HCV
to their sex partner.
- Women who are HCV-infected and wish to have children should
discuss their choices beforehand with a medical specialist.
People with HCV should not donate blood, semen or body organs.
Currently there are two approved antiretroviral treatments
for HCV. The cost of the treatments can be high, and the side
effects can be significant (fatigue, flu-like symptoms, nausea,
depression and anemia). People infected with HCV should abstain
from alcohol use, as this can further damage the liver.
Many people who are infected with HCV are unaware of their
status. People who should consider testing are:
- Current or former injection drug users.
- Persons who received blood transfusions or an organ transplant
prior to May 1992.
- Hemophiliacs who received clotting factor concentrates
produced before 1987.
- Persons who have received chronic hemodialysis.
- Infants born to infected mothers.
- Healthcare workers who have been occupationally exposed
to blood or who have had accidental needlesticks.
- Persons who are sex partners of people with HCV.
Testing for HCV is available through physicians and some
health departments.
HIV/HCV Coinfection
Many people who become infected with HIV from injection drug
use are already infected with HCV. Some estimate that 40%
of HIV-infected people in the U.S. are also infected with
HCV. People who are co-infected with both viruses and have
immune system impairment, may progress faster to serious,
chronic or fatal liver damage.
Most new HCV infections in the U.S. are among injecting drug
users. The majority of hemophiliacs who received blood products
contaminated with HIV also are infected with HCV. Treating
HIV in someone with HCV may be complicated, because many of
the medicines that are used to treat HIV may damage the liver.
Continue on to Psychosocial
Issues/Stigma
|